For millions of people worldwide, the simple act of walking, climbing stairs, or kneeling is a painful ordeal. Knee osteoarthritis (OA), the wear-and-tear disease that degrades the cartilage cushioning our joints, is a leading cause of disability. Traditionally, the treatment roadmap has been grim: start with painkillers and physical therapy, move to steroid injections, and eventually, submit to the major surgery of a total knee replacement. It is a management strategy, not a cure.
However, a new frontier in orthopedics is emerging, promising not only to manage symptoms but also to reverse damage potentially. Stem Cell Therapy—a form of regenerative medicine—is captivating both patients and researchers. By harnessing the body’s own repair mechanisms, this therapy aims to reduce inflammation, heal damaged tissue, and delay or prevent the need for metal and plastic implants.
This article examines the science, procedures, evidence, and reality of knee stem cell therapy, separating hype from hope.
Understanding the Problem: The Degenerating Knee
To appreciate the solution, we must understand the failure. The knee is a hinge joint protected by articular cartilage—a smooth, white tissue that covers the ends of your bones. It allows for frictionless movement. Over time, due to aging, injury, or genetics, this cartilage degenerates.
Unlike skin or bone, cartilage has no blood supply. It cannot heal itself. Once it frays, the body’s attempt to repair it often leads to inflammation, bone spurs, and pain. This is Osteoarthritis. Standard treatments (NSAIDs, cortisone) act as band-aids; they reduce pain but do nothing to stop the cartilage from deteriorating further.
The Promise of Stem Cells: Nature’s Repair Kit
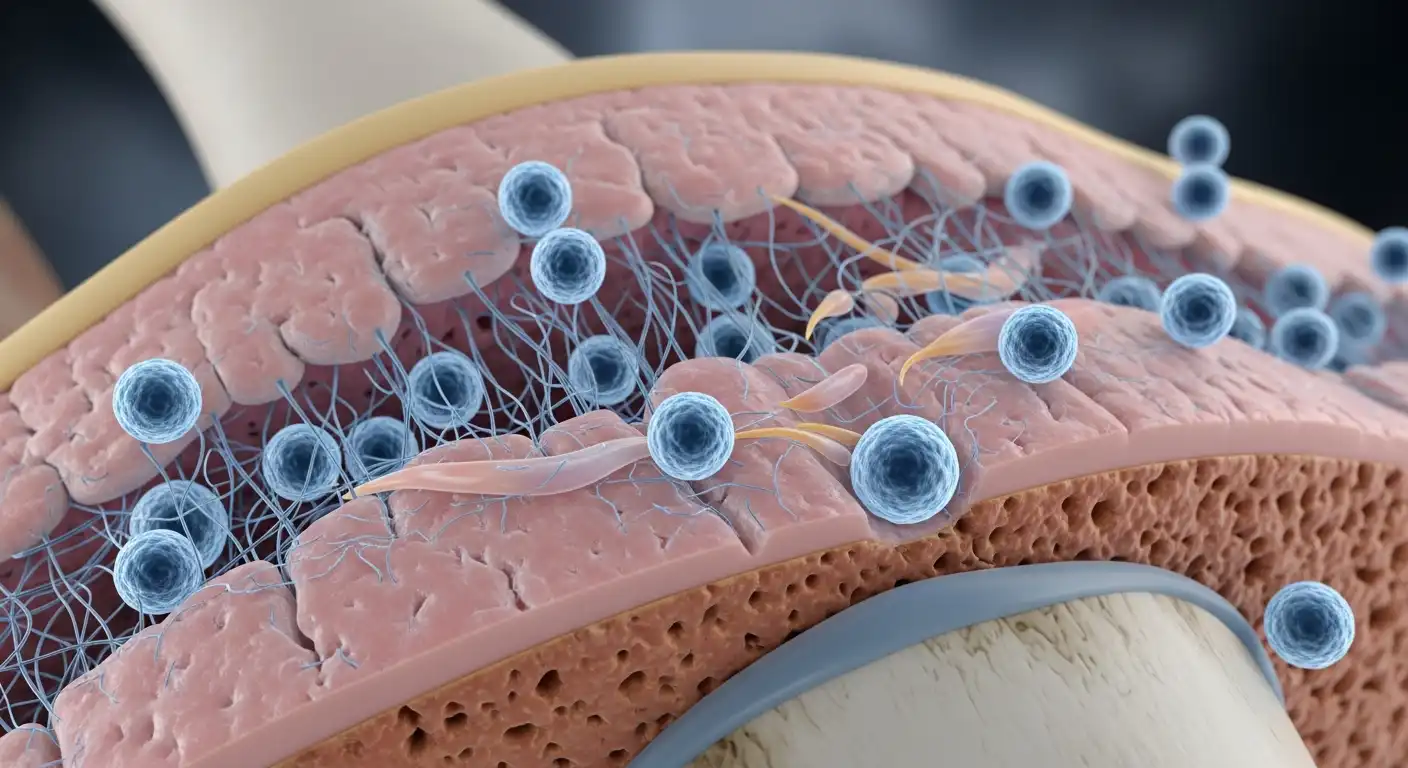
Stem cells are the body’s raw materials. They are unspecialized cells capable of self-renewal through cell division and, under certain physiological or experimental conditions, can be induced to become tissue- or organ-specific cells.
In orthopedics, we primarily focus on Mesenchymal Stem Cells (MSCs). These are adult stem cells found in bone marrow, fat tissue, and synovial fluid. They are unique because they can differentiate into:
- Chondrocytes (Cartilage cells)
- Osteoblasts (Bone cells)
- Adipocytes (Fat cells)
The Mechanism of Action: More Than Just “Regrowth”
Early marketing suggested that if you injected stem cells into a knee, they would magically turn into new cartilage and fill the potholes. We now know the science is more complex and subtle. The primary benefit of MSCs appears to be paracrine signaling.
Think of stem cells less as “seeds” and more as “general contractors.” When injected into a hostile environment (an arthritic knee), they release bioactive molecules (cytokines and growth factors). These signals:
- Reduce Inflammation: They effectively suppress the chronic inflammation that degrades the joint.
- Modulate the Immune System: They stop the body from attacking its own tissue.
- Prevent Cell Death: They protect existing cartilage cells from dying (apoptosis).
- Stimulate Repair: They recruit the body’s resident repair cells to initiate repair.
While some actual cartilage regeneration may occur, the dramatic pain relief patients often experience is primarily due to the massive anti-inflammatory effect that alters the knee’s internal environment.
Sources of Stem Cells: Where Do They Come From?
Not all stem cell treatments are created equal. The source of the cells is critical to safety, efficacy, and regulatory considerations.
Autologous Bone Marrow Aspirate Concentrate (BMAC)
This is the “gold standard” in current clinical practice.
- The Procedure: The doctor numbs the posterior aspect of the patient’s hip (iliac crest) and uses a needle to aspirate bone marrow.
- Processing: This blood is centrifuged to concentrate stem cells and growth factors.
- Injection: The concentrate is injected immediately into the patient’s knee.
- Pros: It uses your own cells (no rejection risk), is FDA-compliant (minimal manipulation), and has the most research backing it.
Adipose-Derived Stem Cells (Fat)
Regenerative cells harvested from a small liposuction of abdominal or flank fat constitute a rich source of mesenchymal stem cells that may help reduce inflammation and support tissue repair in knee osteoarthritis.
- The Procedure: A mini-liposuction is performed on the belly or flank to harvest fat.
- Processing: The fat is processed to separate the stem cells from the oil and tissue.
- Pros: Fat contains significantly more MSCs per volume than bone marrow.
- The Regulatory Hurdle: In the US, the FDA has strict rules about “minimal manipulation.” Treating fat with enzymes to isolate cells (creating Stromal Vascular Fraction, or SVF) is currently considered creating a “drug,” making it subject to strict regulation. Many clinics use mechanical emulsification (chopping the fat) to stay compliant.
Allogeneic Cells (Birth Tissue)
These cells are obtained from a donor, typically from amniotic fluid, placental tissue, or umbilical cord blood collected after a healthy C-section birth.
- Pros: No painful harvest procedure for the patient; “younger” cells might be more potent.
- The Controversy: Research has shown that many commercial “amniotic stem cell” vials contain no viable stem cells by the time they are thawed in a physician’s office. They are essentially growth factor soups. While they can help with inflammation, marketing them as “live stem cell therapy” is often misleading.
The Evidence: What Do the Studies Say?
Is this snake oil, or is it science? The answer lies in the middle, leaning toward promising science.
- Pain Relief: Multiple meta-analyses (studies of studies) have shown that MSC injections provide statistically significant pain relief and improved function for patients with mild to moderate Knee OA, often lasting 6 to 12 months, sometimes longer.
- Cartilage Regrowth: Evidence for the growth of thick new cartilage on MRI scans is limited. While some studies show stabilization of cartilage loss, patients expecting a “brand new knee” will be disappointed.
- Comparison to Steroids: Studies suggest that while steroids offer quick relief that fades in weeks, stem cells take longer to work (weeks to months), but the relief lasts much longer (a year or more).
The Verdict: It is an effective biological therapy for symptom management and potentially slowing disease progression, but it is not yet a guaranteed “cure” for bone-on-bone arthritis.
The Patient Journey: What to Expect
If you decide to pursue this therapy, here is the typical process.
Candidacy
You are likely a good candidate if:
- You have mild-to-moderate osteoarthritis (Grade 2 or 3).
- You want to delay or avoid knee replacement surgery.
- You have failed conservative treatments (PT, NSAIDs).
You are likely not a good candidate if:
- You are “bone-on-bone” (Grade 4) with severe deformity. (Though it may still help pain, it won’t fix the mechanics).
- You have active cancer or an infection.
- You have a bleeding disorder.
The Procedure Day
The treatment is typically an outpatient procedure that takes 2-3 hours.
- Harvest: The bone marrow or fat is collected (usually under local anesthesia).
- Preparation: You wait for 20-30 minutes while the lab processes the cells.
- Injection: The doctor uses Ultrasound or Fluoroscopic (X-ray) guidance to ensure the needle enters the joint space precisely. Blind injections (without imaging) frequently miss the joint and should be avoided.
Recovery
The recovery phases are discussed below:
- Phase 1 (Days 1-3): The knee will be sore and swollen. This is a normal inflammatory response—the cells are “waking up” the area. Ice and rest are key. Nonsteroidal anti-inflammatory drugs (NSAIDs; Advil/Aleve) are usually strictly prohibited because they blunt the stem cell effect.
- Phase 2 (Weeks 2-6): Most patients start to feel improvement.
- Phase 3 (Months 3-6): Peak benefit is usually observed.
The Cost and Insurance Reality
This is the biggest barrier. In the United States and most of Europe, stem cell therapy for arthritis is considered investigational. This means insurance companies, including Medicare, do not cover it.
- Cost: Patients pay out of pocket. Prices vary widely depending on the clinic and cell source, typically ranging from $3,000 to $6,000 per knee.
- Value Proposition: Patients must weigh this cost against the deductibles, time off work, and copays associated with a knee replacement surgery (which can cost insurers $30,000+).
Risks and Red Flags: Navigating the Wild West
The regenerative medicine field has been dubbed the “Wild West” because marketing often outpaces science. While the procedure is generally safe (low risk of infection or reaction since it’s your own cells), there are financial and efficacy risks.
Red Flags to Watch For:
- “Guaranteed” Results: No ethical doctor guarantees a medical outcome.
- “One Magic Vial Treats Everything”: Clinics claiming IV stem cells cure everything from Alzheimer’s to Autism to Arthritis should be avoided. Knee OA requires a localized injection.
- Seminars in Hotels: High-pressure sales tactics at free dinner seminars are a hallmark of predatory clinics.
- No Imaging: If the doctor doesn’t use ultrasound or X-ray to guide the needle, walk away.
- Chiropractic/Nurse Practitioner Clinics: While these providers are valuable, stem cell harvest and injection are complex medical procedures ideally performed by an Orthopedic Surgeon, Sports Medicine Physician, or Pain Management Specialist.
The Future: Moving Toward Standardization
The future of stem cell therapy lies in “Ag-MSCs” (Agitated/Activated MSCs) and gene-edited cells. Researchers are working on:
- Off-the-shelf Allogeneic Cells: Developing universal donor cells that are rigorously tested and potent, removing the need for painful bone marrow harvests.
- Scaffolding: Combining stem cells with 3D-printed bio-scaffolds that provide a structure for the cartilage to grow on, improving the chances of true regeneration.
- Exosomes: These are the tiny vesicles (“bubbles”) that stem cells release to send signals. Some researchers believe that injecting just the exosomes (the signal) without the cell might be safer and just as effective.
Conclusion
Stem cell therapy for knee osteoarthritis represents a paradigm shift from “replacing” parts to “restoring” them. For the active patient in their 40s, 50s, or 60s who isn’t ready for a metal knee, it offers a compelling, though expensive, bridge.
It is not magic. It will not grow you a teenage knee. However, for many, it reduces the perception of pain, improves function, and buys valuable time. As clinical trials continue and the technology refines, regenerative medicine may one day make the total knee replacement a procedure of the past. Until then, educated optimism is the best prescription.